AI's Role in Early Cancer Detection
Artificial intelligence (AI) is rapidly transforming various fields, and oncology is no exception. AI-powered systems are demonstrating significant potential in assisting with early cancer detection, a crucial aspect of successful treatment. By analyzing complex medical images like X-rays, CT scans, and MRIs, AI algorithms can identify subtle patterns and anomalies that might be missed by the human eye. This capability allows for earlier diagnosis, potentially leading to more effective interventions and improved patient outcomes.
One of the key advantages of AI in this context is its ability to process vast amounts of data with remarkable speed and accuracy. Medical professionals often face a deluge of information, making it challenging to meticulously review every image and piece of patient data. AI algorithms can sift through this data, highlighting potential indicators of cancer, freeing up clinicians to focus on the most critical cases and providing them with valuable insights to guide their decision-making process. This streamlined approach to data analysis can significantly expedite the diagnostic process, which is often a critical factor in determining the best course of treatment.
Furthermore, AI algorithms can be trained on large datasets of cancer images and patient records, allowing them to learn and adapt to different types of cancers and their unique characteristics. This constant learning process enhances the accuracy of AI-driven diagnostics over time, leading to more reliable and precise detection of cancerous tissues. The ability to continually refine and improve AI models is crucial for optimizing their effectiveness in complex medical scenarios.
Personalized Cancer Treatment Strategies Through AI
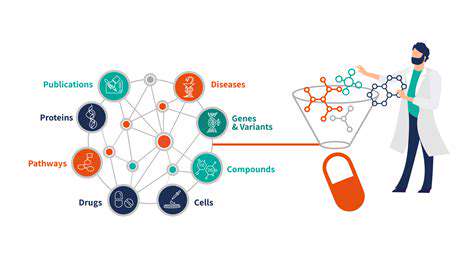
Beyond early detection, AI is also playing a pivotal role in personalizing cancer treatment strategies. By analyzing a patient's unique genetic profile, medical history, and tumor characteristics, AI algorithms can identify the most effective treatment options, minimizing potential side effects and maximizing treatment efficacy. This personalized approach to cancer care is revolutionizing the field, moving away from one-size-fits-all treatments towards tailored interventions specific to each patient's needs.
AI can help predict a patient's response to different therapies. By considering a multitude of factors, including tumor genetics, immune system responses, and patient demographics, AI algorithms can generate personalized treatment plans. This capability enables oncologists to choose therapies that are more likely to be effective and reduce the risk of adverse reactions. This level of precision in treatment selection is crucial for improving outcomes and minimizing the burden on patients.

Improving Patient Outcomes and Experience
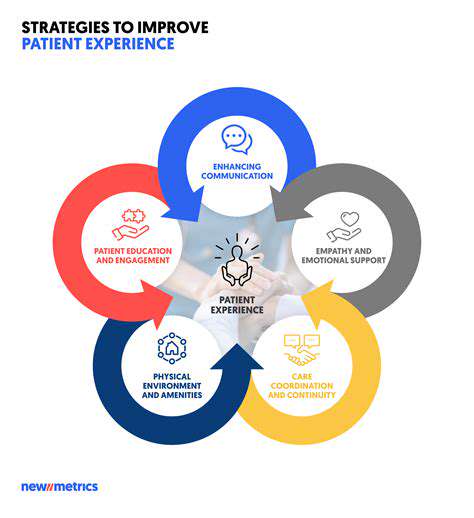
Improving Patient Engagement
Patient engagement is a critical component of achieving positive health outcomes. By actively involving patients in their own care, healthcare providers can foster a more collaborative and effective relationship. This engagement extends beyond simply following instructions; it involves empowering patients to take an active role in their health journey, making informed decisions, and actively participating in their treatment plans. This proactive approach can lead to better adherence to prescribed medications and therapies, ultimately contributing to improved health outcomes. Patients who feel heard and respected are more likely to be motivated to actively participate in their care, leading to better health outcomes.
Furthermore, patient engagement can lead to a more holistic understanding of the patient's needs and preferences. Gathering feedback and actively listening to patient concerns can help healthcare providers tailor treatment plans to individual circumstances, promoting greater patient satisfaction and compliance. This individualized approach is essential for optimizing the effectiveness of interventions and ultimately improving the overall patient experience. By fostering a sense of shared responsibility and decision-making, patient engagement can transform the healthcare experience from a passive transaction to an active partnership, ultimately benefiting both the patient and the healthcare system.
Optimizing Communication Strategies
Effective communication is paramount in achieving positive patient outcomes. Clear and concise communication between healthcare providers and patients is essential for ensuring that patients understand their conditions, treatment options, and potential risks. This includes using plain language, avoiding medical jargon, and actively encouraging questions and concerns. It's crucial for patients to feel comfortable asking questions and expressing their needs without feeling intimidated or pressured.
A key element of optimal communication involves active listening and empathy. Healthcare providers should strive to understand patients' perspectives, concerns, and cultural backgrounds. Empathetic communication fosters trust and rapport, making patients more receptive to information and advice. This approach not only improves understanding but also promotes a supportive environment where patients feel empowered to actively participate in their care, ultimately leading to improved outcomes.
Integrating various communication methods, such as telehealth platforms, patient portals, and regular check-ins, can further enhance the effectiveness of communication. By providing multiple avenues for interaction, healthcare providers can ensure that patients have access to the information and support they need, regardless of their location or circumstances. This comprehensive approach not only improves the quality of care but also enhances the patient experience overall.
Open and honest communication promotes trust, empowering patients to actively participate in their healthcare journey. This active participation is fundamental to achieving optimal health outcomes and ultimately improving the entire patient experience.