Introduction to AI in Patient Triage
Understanding the Basics of AI in Clinical Trials
Artificial intelligence (AI) is rapidly transforming various sectors, including healthcare. Its application in clinical trials is poised to revolutionize the way we conduct research and develop new treatments. AI algorithms can analyze vast datasets, identify patterns, and make predictions that were previously impossible for humans to discern. This allows for more efficient and effective trial design, data analysis, and patient recruitment.
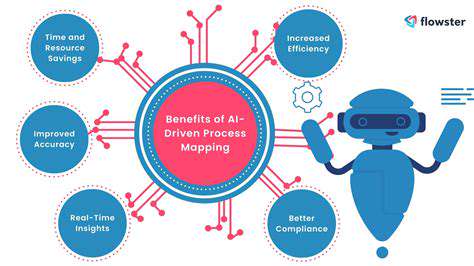
AI can significantly reduce the time and cost of clinical trials by automating various tasks. This acceleration in the drug development process is crucial for bringing life-saving treatments to patients more quickly. Moreover, AI can help identify patients who are most likely to benefit from a specific treatment, leading to more targeted and personalized therapies.
Improving Trial Design and Efficiency
AI tools can optimize trial design by analyzing existing data to identify potential risks and challenges. This allows researchers to tailor protocols, ensuring a more efficient and effective trial process. By simulating different scenarios and predicting outcomes, AI can help researchers make informed decisions about trial size, patient selection criteria, and data collection methods.
This improved efficiency translates to significant cost savings and faster time to market for new therapies. AI-driven insights can also help refine trial protocols, reducing the risk of inefficiencies and improving the chances of success.
Enhanced Data Analysis and Interpretation
AI algorithms excel at processing and analyzing massive datasets from clinical trials. They can identify subtle patterns and correlations that might be missed by human analysts. This ability to unearth hidden insights can lead to a deeper understanding of disease mechanisms and potential treatment targets.
The accuracy and speed of AI-powered data analysis can significantly improve the quality and reliability of clinical trial results. Furthermore, AI can identify potential biases in data collection and analysis, helping to ensure the integrity and validity of research findings.
Personalized Medicine and Patient Selection
AI has the potential to revolutionize patient selection for clinical trials. By analyzing patient data, AI can identify individuals who are most likely to respond favorably to a particular treatment. This targeted approach leads to more efficient use of resources and improves the likelihood of positive outcomes.
This personalization is a major step towards more effective and tailored medical interventions. Furthermore, AI can help identify patients who may experience adverse reactions to a treatment, allowing for proactive risk mitigation.
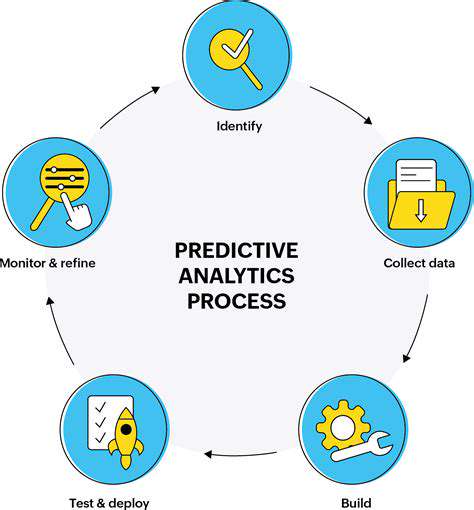
Predictive Modeling for Trial Outcomes
AI-powered predictive models can forecast the likelihood of success for a clinical trial. By analyzing historical data and identifying patterns, AI can provide valuable insights into potential outcomes. This predictive capability allows researchers to make informed decisions about the feasibility and viability of a trial.
This predictive power can guide resource allocation and decision-making, leading to more successful trial outcomes and a greater return on investment. This also allows for adjustments in trial design based on predicted outcomes, optimizing the entire research process.
Ethical Considerations and Future Directions
As AI becomes more integrated into clinical trials, it's crucial to address potential ethical considerations. Ensuring data privacy and security, minimizing bias in algorithms, and maintaining transparency are paramount. Furthermore, establishing clear guidelines and regulations for the use of AI in clinical research is essential.
The future of AI in clinical trials holds immense promise, but it's essential to navigate the ethical challenges with careful consideration. Continued research and development, alongside robust ethical frameworks, will pave the way for responsible and impactful application of AI in patient care and research.
Enhanced Accuracy and Reduced Bias
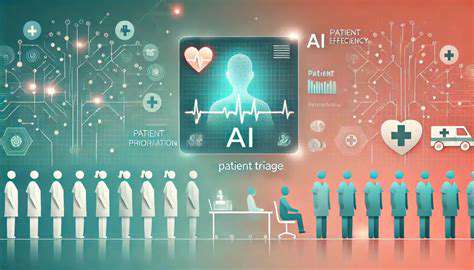
Improved Diagnostic Accuracy
AI algorithms can analyze patient data, including medical history, symptoms, and test results, with significantly greater speed and accuracy than human clinicians. This enhanced diagnostic capability allows for faster identification of critical conditions, leading to quicker interventions and potentially better patient outcomes. By identifying subtle patterns and correlations in data that might be missed by human observation, AI systems can contribute to more precise diagnoses and a more accurate assessment of patient needs.
The ability of AI to analyze vast datasets allows for the identification of patterns and correlations that might be missed by human clinicians. This detailed analysis can lead to more accurate predictions of disease progression and potential complications, enabling proactive interventions and potentially improving patient outcomes.
Minimizing Bias in Prioritization
One significant challenge in traditional patient triage systems is the potential for unconscious bias. Human clinicians, despite their best intentions, may inadvertently prioritize patients based on factors like gender, race, or socioeconomic status. AI systems, trained on large, diverse datasets, can mitigate this bias by focusing solely on objective medical criteria. This objectivity helps ensure that patients receive the most appropriate care based on their individual needs and conditions, rather than on extraneous factors.
Streamlined Patient Flow
AI-powered triage systems can efficiently manage patient arrivals, ensuring that those with the most urgent needs are seen first. This streamlined workflow reduces wait times for critical patients while also optimizing the overall efficiency of the healthcare system. By prioritizing patients based on the severity of their condition, AI algorithms can help healthcare providers allocate resources effectively, further improving the quality of care.
Enhanced Resource Allocation
AI can analyze real-time data to identify trends and patterns in patient needs. This allows healthcare providers to proactively allocate resources, such as beds, personnel, and equipment, to areas where they are most needed. By optimizing resource allocation, AI-powered systems can ensure that resources are utilized effectively, thereby improving the overall efficiency and effectiveness of the triage process.
Data-Driven Decision Making
AI algorithms continually learn and adapt based on the data they process. This iterative learning process allows for continuous improvement in the accuracy and effectiveness of patient prioritization. The resulting data-driven insights can inform decision-making at various levels of the healthcare system, leading to evidence-based strategies for optimizing patient care and resource management. This ongoing refinement of the triage process ensures that systems remain responsive to evolving patient needs and healthcare demands.
The Future of AI in Emergency Care
Improving Diagnostic Accuracy
Artificial intelligence (AI) algorithms are being trained on massive datasets of medical images, patient records, and clinical outcomes to enhance diagnostic accuracy in emergency care. This allows for faster and more precise identification of critical conditions, such as stroke, heart attack, and pneumonia. The potential for AI to analyze data beyond human limitations is significant, leading to earlier interventions and ultimately, better patient outcomes.
By identifying subtle patterns and anomalies, AI can assist in differentiating between similar conditions, enabling quicker and more accurate diagnoses. This is particularly valuable in situations where time is of the essence, like in emergency rooms. The speed and precision of AI-powered diagnostics can drastically improve the chances of survival and recovery in emergency situations.
Personalized Treatment Plans
AI can analyze a patient's individual characteristics, medical history, and current condition to create personalized treatment plans. This includes considering factors such as age, genetics, lifestyle, and pre-existing conditions, leading to more effective and tailored interventions. The ability to customize treatment plans can significantly improve patient outcomes by addressing specific needs and vulnerabilities.
Enhanced Triage and Resource Allocation
AI can be used to optimize triage processes, allowing emergency medical personnel to prioritize patients based on the severity of their condition and the availability of resources. This ensures that patients requiring immediate attention receive it promptly. This can significantly reduce wait times for critical care and improve the overall efficiency of emergency departments.
Furthermore, AI can predict resource needs, such as the number of beds, staff, and specialized equipment required, enabling proactive resource allocation. This proactive approach helps emergency departments prepare for potential surges in patient volume and optimize the utilization of resources.
Predictive Modeling for Risk Assessment
AI models can analyze patient data to predict the risk of certain medical complications, enabling proactive interventions and potentially preventing adverse events. This can assist in identifying patients at high risk for complications and allowing for preventative measures to be put in place. Predictive models can also assist in identifying patients who may need more intensive monitoring or specialized care.
Remote Patient Monitoring and Early Detection
AI-powered wearable devices and remote monitoring systems can continuously track vital signs and other health parameters. This allows for early detection of potential health issues before they escalate into critical emergencies. This proactive approach can significantly improve the chances of successful interventions and reduce the severity of complications.
Improved Communication and Collaboration
AI can facilitate seamless communication and collaboration between healthcare professionals, enabling faster information sharing and more coordinated care. This can involve real-time data transmission, automated alerts for critical conditions, and improved communication between different departments within a hospital or across healthcare systems. The improved communication and collaboration can expedite the decision-making process and ultimately lead to better patient outcomes.
Ethical Considerations and Regulations
The increasing use of AI in emergency care raises important ethical considerations regarding data privacy, algorithmic bias, and the responsibility of AI systems. Establishing clear ethical guidelines and regulations will be crucial to ensure that AI is used responsibly and equitably in emergency settings. Careful consideration must be given to the potential for bias in algorithms and the need for transparency in decision-making processes. Ensuring patient data privacy is paramount, and robust safeguards need to be implemented to prevent misuse.