Improving Efficiency and Accessibility

Streamlining Workflow Processes
Efficient workflow processes are crucial for any organization aiming to improve productivity and reduce operational costs. By identifying and eliminating bottlenecks in existing processes, organizations can significantly increase the speed and accuracy of task completion. This involves analyzing current workflows, identifying areas for improvement, and implementing solutions that streamline the steps required to complete a task. This process often necessitates the adoption of new technologies or the re-evaluation of existing methods.
Optimizing Resource Allocation
Effective resource allocation is paramount to maximizing efficiency and productivity. This involves strategically assigning resources, including personnel, equipment, and materials, to specific tasks based on their capabilities and requirements. Proper resource allocation minimizes wasted effort and ensures that tasks are completed efficiently and on time. Careful planning and monitoring of resource utilization are essential for achieving optimal results.
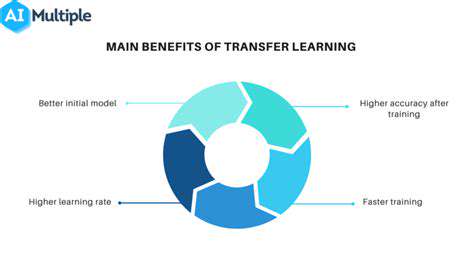
Leveraging Technology for Automation
Technology plays a vital role in improving efficiency. Automation of repetitive tasks can free up valuable employee time for more complex and strategic work. Implementing automation tools can significantly increase productivity and reduce the risk of errors. By automating certain processes, organizations can reduce operational costs and improve overall efficiency.
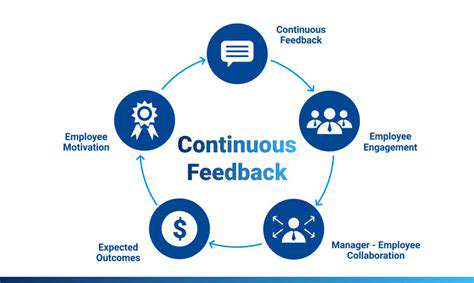
Enhancing Communication Channels
Clear and effective communication is essential for successful collaboration and coordination. Establishing clear communication channels and protocols ensures that information is disseminated quickly and accurately, minimizing misunderstandings and delays. This includes utilizing various communication tools such as instant messaging, video conferencing, and project management software. Improved communication also fosters a sense of teamwork and shared responsibility within the organization.
Prioritizing Training and Development
Investing in employee training and development is a crucial aspect of enhancing efficiency and accessibility. Providing employees with the necessary skills and knowledge to perform their tasks effectively directly impacts productivity and overall performance. This can involve offering workshops, online courses, or mentoring programs. A well-trained workforce is better equipped to handle challenges and contribute to the organization's success.
Ensuring Accessibility for Diverse Needs
Accessibility should be a key consideration in all processes and procedures. Making sure that all employees, regardless of their abilities or disabilities, have equal access to information and resources is vital for creating a truly inclusive and equitable work environment. This involves adapting workflows, technologies, and communication methods to accommodate diverse needs, ensuring that everyone can participate fully and contribute their skills. It is crucial to incorporate diverse perspectives in all stages of the process.
Improving Data Management Practices
Effective data management is crucial for decision-making and informed strategy development. By establishing clear data collection, storage, and retrieval procedures, organizations can improve their ability to analyze performance, identify trends, and make informed decisions. This involves implementing robust data management systems, ensuring data security, and training personnel on best practices for data handling. Accurate and readily available data is essential for optimizing processes and achieving desired outcomes.
Ethical Considerations and Future Directions
Data Privacy and Security
Protecting patient data is paramount in AI-driven physical medicine and rehabilitation. Robust security measures are crucial to prevent unauthorized access, breaches, and misuse of sensitive information. This includes anonymization techniques, encryption protocols, and adherence to stringent data privacy regulations like HIPAA in the US and GDPR in Europe. Failing to prioritize data security can have severe consequences, ranging from reputational damage to legal repercussions. Implementing strong access controls, regular security audits, and educating healthcare professionals about data protection best practices are essential steps in ensuring patient trust and compliance.
Furthermore, clear guidelines and consent protocols must be established for the collection, storage, and utilization of patient data. Patients should be informed about how their data will be used, and they must have the right to access, correct, and delete their information. Transparency and patient empowerment are key elements in building trust and fostering ethical AI implementation in physical rehabilitation.
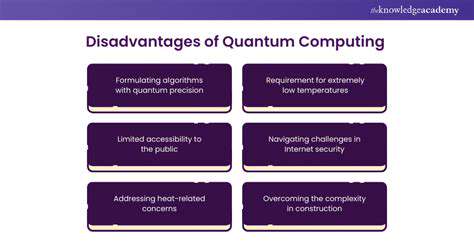
Bias and Fairness in AI Algorithms
AI algorithms are trained on data, and if that data reflects existing societal biases, the resulting algorithms can perpetuate and even amplify those biases. This can lead to unequal access to care, disparities in treatment outcomes, and potentially discriminatory practices in physical rehabilitation. For instance, if a dataset used to train an AI system for gait analysis disproportionately represents individuals of a certain age or demographic group, the AI may not accurately assess the gait of others, potentially leading to suboptimal treatment plans. Therefore, rigorous testing for bias and ongoing monitoring of AI algorithms are critical to ensure fairness and equity in their application to physical medicine and rehabilitation.
Careful consideration must be given to the diverse populations being served. AI models should be evaluated across different demographics to identify and mitigate potential biases in their assessments and recommendations. Continuous monitoring and adaptation of the algorithms are necessary to address evolving societal needs and ensure equitable outcomes.
Transparency and Explainability
Understanding how AI algorithms arrive at their conclusions is critical for building trust and ensuring accountability. Black box algorithms, where the decision-making process is opaque, can be problematic in healthcare settings where clinicians need to understand the reasoning behind treatment recommendations. In physical rehabilitation, explainable AI (XAI) techniques are vital for clinicians to comprehend the factors influencing an AI's assessment of a patient's condition and treatment plan. This transparency facilitates better collaboration between AI systems and human practitioners, allowing for a more holistic and informed approach to patient care.
Clinical Validation and Rigorous Testing
AI systems used in physical medicine and rehabilitation must undergo rigorous clinical validation to ensure their accuracy and effectiveness. This involves testing the AI's performance against established clinical standards and benchmarks, and comparing its results to those obtained through traditional methods. These validation processes need to be transparent and well-documented to demonstrate the reliability and safety of the AI in real-world applications. Furthermore, ongoing monitoring and evaluation of AI performance in real-world clinical settings are crucial for continuous improvement and adaptation.
Human-AI Collaboration and Roles
AI should augment, not replace, human clinicians. The future of physical medicine and rehabilitation likely lies in a collaborative relationship between AI systems and healthcare professionals. AI can handle tasks such as data analysis, image processing, and identifying potential issues, enabling clinicians to focus on complex cases, patient interaction, and nuanced decision-making. Establishing clear guidelines about the roles and responsibilities of both humans and AI systems is essential to ensure a smooth and effective integration. This includes training programs for healthcare professionals to develop the skills needed to effectively work alongside AI tools.
Ethical Oversight and Regulation
Establishing clear ethical guidelines and regulatory frameworks for the development and deployment of AI in physical medicine and rehabilitation is essential. These frameworks should address issues such as data privacy, algorithm bias, transparency, and accountability. Collaboration between researchers, clinicians, policymakers, and ethicists is crucial for creating responsible guidelines that prioritize patient safety, well-being, and equitable access to care. This includes the creation of oversight bodies to monitor the ethical implementation and impact of AI in this field.
Societal Impact and Accessibility
The implementation of AI in physical medicine and rehabilitation should consider its potential societal impact. Ensuring equitable access to AI-powered tools and services across different socioeconomic groups is vital. This requires careful consideration of affordability, accessibility, and the potential for exacerbating existing health disparities. Furthermore, public education and awareness campaigns are necessary to foster trust and understanding of AI's role in improving physical rehabilitation outcomes for all.