Optimizing Healthcare Delivery Through Real-Time Monitoring
Streamlining Processes for Enhanced Efficiency
Optimizing healthcare delivery hinges on streamlining various processes, from patient intake to appointment scheduling and post-discharge follow-up. This involves leveraging technology to automate administrative tasks, reducing manual data entry and freeing up valuable clinician time. By automating these processes, healthcare providers can focus more on patient care and less on administrative burdens. This enhanced efficiency can lead to reduced wait times, improved patient satisfaction, and ultimately, better health outcomes. Furthermore, streamlining processes can help identify areas for improvement and foster a more collaborative environment within the healthcare team.
Implementing robust electronic health record (EHR) systems is crucial for efficient data management and accessibility. These systems allow for seamless information sharing among healthcare professionals, facilitating better coordination of care and reducing the risk of medical errors. A well-implemented EHR system can also support proactive care management, allowing for early identification of potential health issues and timely interventions. This proactive approach can significantly impact patient outcomes and reduce the need for expensive and potentially harmful emergency interventions.
Improving Access and Affordability
A key component of optimizing healthcare delivery involves expanding access to care, particularly for underserved populations. This might involve implementing telehealth programs, expanding clinic hours, or establishing mobile health units in remote areas. These initiatives can significantly increase accessibility to critical healthcare services for individuals who might otherwise face significant challenges in accessing care.
Another crucial aspect is addressing the cost of healthcare. This involves exploring innovative payment models, such as value-based care, which incentivizes providers to focus on preventative care and improved patient outcomes. Value-based care can potentially lead to significant cost savings in the long run while ensuring high-quality care. Additionally, exploring alternative care delivery models, such as community health centers and patient navigation programs, can help lower the financial burden on patients, making healthcare more affordable and accessible to a wider range of individuals.
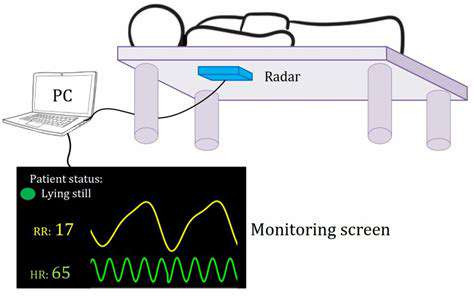
Telehealth is a rapidly evolving solution that can improve access to care for many. By leveraging virtual consultations and remote monitoring, telehealth can extend care to patients in geographically remote areas or those with mobility limitations. This can also reduce travel costs and time commitments for patients, making healthcare more convenient and accessible. Furthermore, telehealth can provide timely follow-up care, reducing the risk of delayed diagnoses and improving overall health outcomes.
Addressing the cost of healthcare is essential to improving accessibility. Exploring innovative payment models, such as value-based care, can incentivize providers to focus on preventative care and improved patient outcomes. This shift can lead to significant long-term cost savings while ensuring high-quality care. Exploring alternative care delivery models, such as community health centers and patient navigation programs, can also help lower the financial burden on patients.
Ultimately, optimizing healthcare delivery requires a multifaceted approach that considers both the efficiency of processes and the affordability and accessibility of care. By combining innovative technology with proactive strategies, healthcare systems can deliver better outcomes for all patients.