Introduction to AI-Powered Disease Surveillance
Early Detection and Prevention
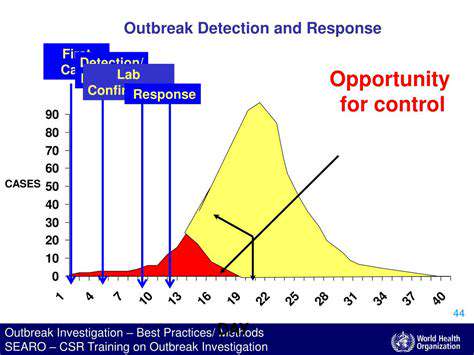
AI-powered disease surveillance systems offer a powerful tool for early detection of outbreaks. By analyzing vast datasets, including patient records, environmental factors, and social media trends, these systems can identify potential patterns and anomalies that might indicate the emergence of a disease. This early detection allows for swift interventions and public health measures, potentially preventing wider outbreaks and mitigating their impact on communities.
The ability to predict potential outbreaks before they manifest is a significant advantage. This predictive capability allows for proactive measures, such as targeted public health campaigns, increased testing, and resource allocation, minimizing the severity and spread of infectious diseases.
Data Integration and Analysis
A key aspect of effective AI-powered disease surveillance is the ability to integrate and analyze diverse data sources. This encompasses integrating patient data from various healthcare systems, environmental data from weather stations and satellite imagery, and social media data to identify potential trends and patterns. Sophisticated algorithms are crucial for processing and analyzing this complex data, identifying correlations, and generating actionable insights.
The integration of diverse data sources allows for a more comprehensive understanding of disease dynamics. For example, analyzing weather patterns alongside reported cases can reveal correlations that may not be apparent through traditional epidemiological methods. This holistic approach leads to a more accurate and nuanced understanding of disease spread and patterns.
Real-time Monitoring and Alerting
AI algorithms can be designed to monitor disease trends in real-time, providing near-instantaneous alerts when anomalies or suspicious patterns emerge. This real-time monitoring allows public health officials to respond promptly to potential outbreaks, activating containment strategies and implementing necessary public health measures, potentially limiting the impact on the community.
The speed and efficiency of real-time monitoring are critical in disease outbreak response. Rapid identification and reporting of potential outbreaks allow for swift action, potentially saving lives and preventing further spread, particularly in the case of highly contagious diseases.
Improved Accuracy and Efficiency
AI algorithms can process vast amounts of data significantly faster and more accurately than traditional methods, leading to improved efficiency in disease surveillance. This enhanced efficiency allows for more comprehensive analysis of disease patterns and trends, leading to more accurate predictions and insights.
Enhanced Public Health Response
The insights derived from AI-powered disease surveillance systems can significantly enhance public health responses. By providing real-time data and predictive models, these systems empower public health officials to make well-informed decisions about resource allocation, public health campaigns, and intervention strategies. This proactive approach leads to more effective and efficient responses, minimizing the impact of outbreaks.
The ability to tailor public health interventions based on real-time data is critical. Using AI to understand disease spread patterns allows for targeted interventions, maximizing the impact of public health resources and minimizing the overall impact of the outbreak.
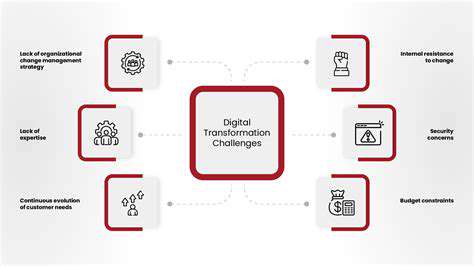
Ethical Considerations and Challenges
While AI-powered disease surveillance presents significant advantages, it also raises ethical concerns regarding data privacy, bias in algorithms, and the potential for misuse of sensitive information. Careful consideration and robust safeguards are necessary to ensure responsible implementation and address potential biases in the data or algorithms used.
Maintaining data security and privacy is paramount in the development and deployment of AI-powered disease surveillance systems. Ensuring patient confidentiality and adhering to strict ethical guidelines are crucial for building trust and mitigating potential risks associated with the use of sensitive health information.
Enhancing Disease Reporting and Communication
Improving Data Collection Practices
Accurate and comprehensive disease reporting hinges on robust data collection methods. These methods must be standardized and consistently applied across all reporting channels to ensure that crucial information isn't overlooked or misrepresented. This includes clear definitions for disease classifications and standardized procedures for collecting patient information, such as medical history, symptoms, and test results. Implementing these robust practices is fundamental to effective disease surveillance and response.
Furthermore, utilizing technology to streamline data entry and storage is crucial. Electronic health records (EHRs) and dedicated disease surveillance systems can significantly reduce manual errors, improve data accessibility, and facilitate timely analysis, thereby enhancing the overall quality and reliability of the collected information. This technological advancement is essential for accurate and efficient disease reporting.
Strengthening Surveillance Systems
Current surveillance systems need enhancements to effectively identify disease trends and outbreaks. This includes expanding surveillance networks to encompass a wider range of healthcare providers and communities, thereby capturing a more comprehensive picture of disease patterns. Early detection and rapid response are crucial in mitigating the impact of emerging health threats.
Improving data analysis capabilities is also key. Sophisticated analytical tools can identify subtle patterns and correlations that might be missed by traditional methods. These tools can help predict outbreaks, identify high-risk populations, and ultimately inform public health interventions.
Enhancing Communication and Collaboration
Effective communication channels are essential for disseminating critical information to healthcare professionals, public health officials, and the public. This includes establishing clear protocols for sharing data and alerts, ensuring that information is disseminated in a timely and accessible manner. This is crucial for coordinating responses to outbreaks and preventing the spread of disease.
Strong collaboration between different stakeholders, including healthcare providers, public health agencies, and research institutions, is paramount. This collaboration allows for a more comprehensive understanding of disease trends, facilitating the development of targeted interventions and strategies to control the spread of diseases. Joint efforts and data sharing are critical in achieving a cohesive response to health crises.
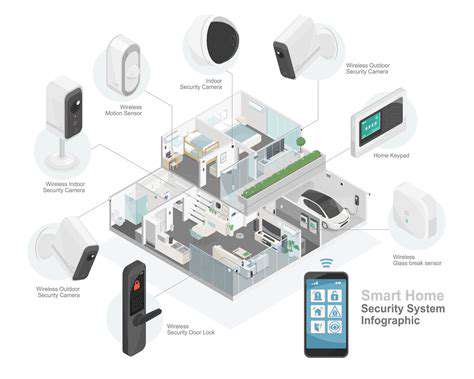
Improving Data Accessibility and Interoperability
Data accessibility is crucial for effective disease reporting. Public health agencies and researchers need seamless access to relevant data, enabling them to conduct thorough analyses and make informed decisions. This includes establishing clear protocols for data sharing, ensuring data privacy and security, and enabling interoperability between different data systems. Improving data accessibility is vital in supporting research efforts and public health initiatives.
Implementing Robust Reporting Standards
Establishing clear and consistent reporting standards is fundamental to accurate and comparable disease data. These standards should encompass specific criteria for disease classification, data collection methods, and reporting timelines. This ensures that data from different sources can be effectively integrated and analyzed. Clear standards minimize ambiguity and enhance the reliability of the reported data. Consistency in reporting practices is key for identifying patterns and trends in disease outbreaks.
Addressing Data Gaps and Limitations
Identifying and addressing data gaps is crucial for improving disease reporting. This includes assessing the availability and quality of existing data, identifying areas where data collection is lacking, and implementing strategies to fill these gaps. Addressing limitations in data collection and analysis is essential for accurate disease surveillance. Understanding and acknowledging potential biases in the data is equally important in ensuring reliable information. This requires thorough analysis and careful consideration of the potential factors that might influence the accuracy of the data.
The Future of AI in Global Health Surveillance
AI's Role in Disease Diagnosis
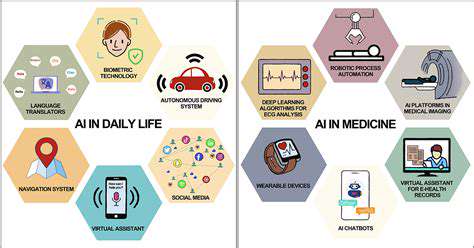
Artificial intelligence (AI) is poised to revolutionize disease diagnosis, offering significant improvements in accuracy and speed. AI algorithms can analyze vast datasets of medical images, patient records, and genetic information to identify patterns and anomalies that might be missed by human clinicians. This capability is particularly valuable in resource-limited settings, where access to specialized expertise is often limited.
Through the use of machine learning, AI can be trained to detect subtle signs of disease, leading to earlier diagnoses and potentially better patient outcomes. This early detection is crucial, as early intervention can significantly improve the chances of successful treatment. The potential for AI to streamline the diagnostic process and improve access to care is immense.
AI-Powered Drug Discovery and Development
AI is rapidly transforming drug discovery and development, accelerating the process and potentially reducing costs. By analyzing massive datasets of chemical compounds and biological information, AI can identify promising drug candidates and predict their potential efficacy and safety. This accelerates the time it takes to bring new treatments to market, a critical factor in addressing global health challenges.
AI can also simulate the effects of drugs on various biological systems, providing insights into potential side effects and interactions. This predictive capability reduces the need for costly and time-consuming animal testing, making the process more ethical and efficient. The potential for AI to revolutionize the development of personalized medicine is substantial.
AI for Personalized Medicine
Personalized medicine, tailoring treatments to individual patient needs, is a promising area where AI can play a significant role. AI can analyze a patient's genetic makeup, lifestyle, and medical history to identify the optimal treatment strategy. This personalized approach can lead to more effective therapies and fewer adverse reactions.
By considering individual variations, AI can help predict treatment responses and tailor dosages to maximize efficacy and minimize side effects. This approach is crucial for improving patient outcomes, especially in complex diseases like cancer.
AI in Public Health Surveillance
AI can significantly enhance public health surveillance systems, enabling faster responses to outbreaks and epidemics. AI algorithms can analyze vast amounts of data, including social media posts, news reports, and epidemiological information, to identify emerging trends and potential outbreaks. This rapid identification allows for timely interventions, limiting the spread of disease.
Predictive modeling based on AI can also help anticipate future outbreaks, enabling proactive measures to prevent their escalation. This capability is critical for global health security, allowing for more effective and timely responses to epidemics.
AI-Driven Health Equity
Addressing health disparities is a crucial aspect of global health. AI has the potential to contribute to reducing these disparities by improving access to care in underserved communities. AI-powered tools can translate medical information, provide remote consultations, and deliver personalized health education, bridging the gap in access.
By targeting interventions to specific populations, AI can enhance the effectiveness of public health initiatives and reduce health inequities. The potential for AI to create a more equitable and accessible healthcare system is undeniable.
Ethical Considerations in AI Healthcare
As AI becomes more integrated into healthcare, ethical considerations become paramount. Ensuring data privacy, algorithmic fairness, and transparency in AI systems is crucial. The use of AI in healthcare must be guided by ethical principles and regulations.
Bias in algorithms can perpetuate existing health disparities, making it essential to address these concerns proactively. Careful consideration of the ethical implications of AI in healthcare is vital to ensure responsible and equitable implementation.
AI and the Future of Healthcare Workforce
The integration of AI in healthcare will undoubtedly reshape the healthcare workforce. AI tools can automate certain tasks, freeing up healthcare professionals to focus on more complex and patient-centric roles. This could lead to a shift in the skills needed within the healthcare workforce.
AI will not replace human clinicians but rather augment their capabilities, enabling them to provide better and more efficient care to patients. The future of the healthcare workforce will involve a collaboration between humans and AI, leading to improved outcomes and a more sustainable healthcare system.