Revolutionizing Diagnostic Precision with AI-Assisted Technologies
Enhancing Diagnostic Capabilities Through Intelligent Systems
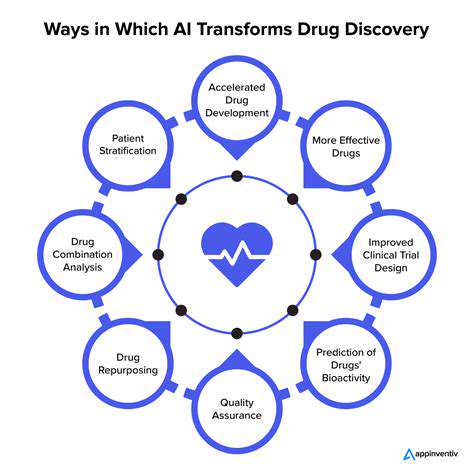
Modern medicine has entered a transformative era with the integration of artificial intelligence into diagnostic processes. Intelligent diagnostic systems now provide unprecedented capabilities for examining comprehensive medical datasets, including imaging studies, electronic health records, and genomic profiles. These advanced tools frequently surpass human practitioners in both processing speed and analytical precision, enabling earlier and more accurate disease identification that directly benefits patient care.
Machine learning algorithms possess a unique capacity to detect subtle pathological patterns that might elude even experienced clinicians. This technological advantage creates opportunities for prompt medical intervention, potentially halting disease progression before severe complications develop.
Advancements in Medical Imaging Interpretation
Contemporary diagnostic systems demonstrate exceptional performance in evaluating radiographic studies, including conventional X-rays, computed tomography, and magnetic resonance imaging. Through meticulous pattern recognition, these tools assist radiologists in achieving higher diagnostic accuracy, minimizing interpretation errors while optimizing workflow efficiency. Such technological support proves particularly valuable in detecting early-stage malignancies, traumatic injuries, and various pathological conditions.
Automated image analysis features allow medical imaging specialists to concentrate on complex diagnostic challenges while maintaining rapid turnaround times. This efficiency gain becomes especially critical in emergency medical situations where timely diagnosis directly impacts patient outcomes.
Predictive Analytics for Preventive Healthcare
Sophisticated analytical models can process comprehensive patient datasets encompassing medical backgrounds, demographic information, and lifestyle factors to forecast disease risk profiles. These predictive capabilities enable healthcare providers to implement targeted preventive measures and customized health management strategies. This proactive approach represents a paradigm shift in population health management, allowing for focused interventions in high-risk patient groups.
By identifying significant data correlations and emerging health trends, intelligent systems empower medical professionals to anticipate potential health issues and optimize therapeutic approaches for diverse patient populations.
Transforming Histopathological Analysis
Digital pathology platforms incorporating machine learning can examine microscopic tissue specimens with remarkable precision, aiding in the identification of malignant cells and other pathological markers. This technological advancement significantly reduces diagnostic timeframes, facilitating prompt treatment decisions that can dramatically affect patient prognosis. The system's ability to recognize subtle cellular alterations often imperceptible to human observers provides a substantial clinical advantage in pathological diagnosis.
Customized Therapeutic Approaches
Modern computational systems can synthesize individual patient data to develop personalized treatment regimens. By integrating genetic profiles, lifestyle considerations, and comprehensive medical histories, these tools recommend optimized therapeutic protocols and medication dosages. This individualized approach minimizes adverse effects while maximizing treatment effectiveness, creating superior patient experiences and improved clinical results.
Navigating Implementation Challenges
While intelligent diagnostic systems offer tremendous potential, significant implementation challenges and ethical considerations must be addressed. Protecting sensitive patient information remains paramount, particularly as these technologies rely on extensive medical datasets. Ensuring algorithmic fairness and reliability across diverse demographic groups represents another critical consideration for equitable healthcare delivery.
Comprehensive testing protocols, continuous performance validation, and transparent operational standards are essential for maintaining system integrity and building public confidence in these advanced diagnostic tools.
Expanding Healthcare Access
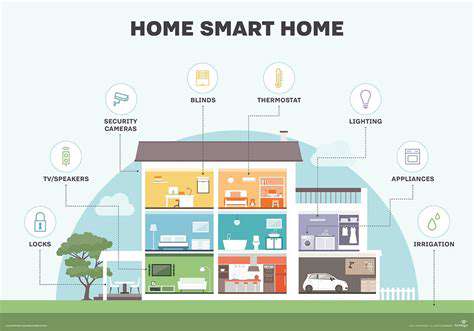
Intelligent diagnostic technologies have the potential to democratize access to advanced medical expertise, particularly in underserved regions with limited healthcare infrastructure. These systems can significantly reduce diagnostic delays and streamline clinical workflows, creating more equitable healthcare access regardless of geographic or socioeconomic barriers. Widespread implementation of these technologies could represent a major advancement in global healthcare accessibility.
Customizing Therapeutic Interventions with Intelligent Systems

Comprehensive Patient Assessment
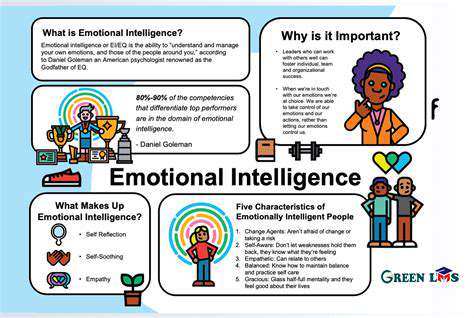
Successful therapeutic interventions require thorough evaluation of each patient's distinctive situation, treatment preferences, and complete medical background. This personalized methodology transcends generic treatment protocols by incorporating critical individual factors such as age, daily routines, economic circumstances, and cultural context. A patient-centered approach that acknowledges and integrates the patient's personal experiences and perspectives proves most effective for achieving sustainable health outcomes.
Particular attention must be given to managing multiple concurrent health conditions, as therapeutic approaches must account for complex interactions between different medical issues. Patients with diabetes mellitus, for instance, require specially tailored management strategies that consider their unique metabolic challenges and potential complications.
Designing Individualized Treatment Plans
Following comprehensive assessment, healthcare providers can develop truly customized intervention strategies. This process involves evaluating various therapeutic options and selecting those most compatible with the patient's specific characteristics and preferences. The optimal treatment plan harmonizes with the patient's lifestyle and personal values, thereby enhancing treatment adherence and improving clinical results. Collaborative decision-making with active patient participation ensures the final plan meets the individual's expectations and needs.
Integrating Patient-Centered Approaches
Successful therapeutic outcomes depend heavily on incorporating patient preferences into treatment planning. Understanding patient priorities, expectations, and preferred communication methods establishes trust and promotes active participation in care. This patient-centered approach involves attentive listening to concerns, thorough explanation of treatment options, and empowering patients to become engaged partners in their healthcare journey.
Treatment delivery methods should also accommodate patient preferences, offering flexible options ranging from traditional in-person consultations to convenient telehealth platforms. Customizing communication styles and service delivery methods enhances patient experience and promotes consistent treatment adherence.
Continuous Treatment Optimization
Personalized medicine represents an ongoing process rather than a single intervention. Regular monitoring and adaptive treatment modifications ensure continued effectiveness as patient circumstances evolve. This requires scheduled follow-up assessments, progress evaluations, and necessary treatment adjustments. Maintaining open communication channels between healthcare providers and patients facilitates timely interventions and prevents potential complications.
Periodic reviews offer valuable opportunities to address emerging challenges or concerns. Continuous treatment adaptation ensures therapeutic strategies remain optimally aligned with the patient's changing health status and life circumstances throughout the care continuum.
Outcome Analysis and Process Improvement
Systematic evaluation of personalized treatment outcomes provides critical insights for refining clinical practices. Collecting and analyzing data on treatment efficacy, patient responses, and satisfaction levels identifies successful strategies and areas for improvement. This evidence-based approach enables continuous refinement of personalized treatment protocols, ensuring ongoing enhancement of patient care quality.
Knowledge sharing among healthcare professionals regarding successful personalization strategies accelerates collective learning and promotes widespread adoption of best practices. This collaborative approach ultimately benefits patients through increasingly effective and individualized healthcare services.