Revolutionizing Elderly Care Through Technology
Technological advancements are profoundly impacting numerous aspects of modern life, and elderly care is no exception. Innovative solutions are emerging, offering unprecedented opportunities to enhance the quality of life for senior citizens. From smart home devices to telehealth platforms, technology is empowering older adults to maintain their independence and well-being while providing crucial support to caregivers.
Personalized Care Plans
The ability to tailor care plans to individual needs is a key benefit of utilizing technology in elderly care. Software applications can analyze various data points, including medical history, lifestyle preferences, and daily routines, to create personalized care plans that address specific requirements. This approach fosters a more responsive and proactive care model, preventing potential issues and promoting overall well-being.
Remote Monitoring and Support
Remote monitoring systems provide caregivers and healthcare professionals with real-time access to vital health information, enabling prompt responses to potential medical emergencies. These systems can track vital signs, medication adherence, and even activity levels, allowing for early intervention and reducing hospital readmissions. This proactive approach can significantly improve the safety and well-being of elderly individuals.
Enhanced Communication and Engagement
Technology facilitates seamless communication between caregivers, family members, and healthcare providers. Video conferencing platforms, messaging apps, and wearable devices allow for constant communication and engagement, fostering a sense of connection and support. This improved communication network is crucial for ensuring that elderly individuals feel supported and involved in their care.
Improving Accessibility and Affordability
Technology has the potential to make elderly care more accessible and affordable for everyone. Telehealth services can reduce the need for in-person visits, lowering travel costs and making consultations more convenient. Furthermore, technology-driven solutions can streamline administrative tasks, reducing costs and improving efficiency for healthcare providers.
Promoting Independence and Dignity
Many elderly individuals desire to maintain their independence and dignity as they age. Smart home devices, such as automated lighting, voice-activated assistants, and safety sensors, empower older adults to live independently in their homes, fostering a sense of security and autonomy. This approach respects the inherent dignity of the individual while promoting a positive aging experience.
Addressing Caregiver Burden
Technology plays a vital role in alleviating the burden on caregivers. Tools designed to track caregiving tasks, share information, and coordinate services can significantly ease the workload for family members and professional caregivers. This support system is essential for ensuring that caregivers have the resources they need to provide effective and sustainable care.
AI-Driven Diagnostics and Monitoring: Early Detection and Proactive Management
Early Disease Detection: Revolutionizing Diagnostics
AI-powered diagnostic tools are rapidly transforming healthcare by enabling early detection of diseases. By analyzing vast datasets of medical images, patient records, and genetic information, AI algorithms can identify subtle patterns and anomalies that might be missed by human clinicians. This early detection is crucial for proactive management, allowing for interventions at earlier stages when treatment options are more effective and the likelihood of positive outcomes is significantly higher.
The potential impact on chronic conditions like diabetes, cardiovascular disease, and cancer is immense. Early detection through AI could lead to significant reductions in morbidity and mortality rates, as well as a substantial decrease in healthcare costs associated with advanced-stage disease management.
Proactive Monitoring and Personalized Treatment Plans
Beyond detection, AI facilitates proactive monitoring of patients' health status. Continuous data collection, analysis, and interpretation can identify potential risks and trigger alerts to healthcare providers, allowing for timely interventions and adjustments to treatment plans.
AI algorithms can also personalize treatment plans by considering individual patient characteristics, genetic predispositions, and response to various therapies. This personalized approach maximizes treatment efficacy and minimizes adverse effects, ultimately leading to improved patient outcomes.
Enhanced Efficiency and Accessibility of Healthcare
AI-driven diagnostic and monitoring systems can significantly enhance the efficiency of healthcare delivery. By automating tasks like image analysis and report generation, AI frees up clinicians' time to focus on patient care and complex cases. This efficiency translates to faster diagnoses, reduced waiting times, and increased access to specialized care, especially in underserved communities.
Improving Accuracy and Reducing Diagnostic Errors
AI algorithms are trained on massive datasets, enabling them to identify patterns and anomalies with a degree of accuracy often exceeding human capabilities. This increased accuracy reduces the risk of misdiagnosis and contributes to more informed treatment decisions. By minimizing errors, AI-driven systems contribute to improved patient safety and better health outcomes.
Ethical Considerations and Future Directions
While AI offers significant promise for advancing healthcare, ethical considerations surrounding data privacy, algorithmic bias, and the role of human clinicians in the diagnostic process need careful attention. Robust regulatory frameworks and ongoing research are crucial to ensure responsible and equitable implementation of AI in healthcare. Ongoing research and development in AI for diagnostics and monitoring will continue to push the boundaries of what's possible, paving the way for even more precise and personalized healthcare in the future.
The future of AI in healthcare is bright. As technology continues to advance, we can anticipate even more sophisticated and effective applications of AI in diagnostics and monitoring, leading to a healthier and more equitable future for all.
Personalized Treatment Plans and Medication Management: Tailoring Care for Individual Needs
Personalized Treatment Plans: A Foundation for Effective Care
Personalized treatment plans are crucial for optimizing health outcomes. They go beyond a one-size-fits-all approach, recognizing that each individual's unique circumstances, medical history, lifestyle, and preferences influence their response to treatment. This tailored approach considers not only the diagnosis but also the patient's overall well-being, enabling clinicians to create a treatment strategy that is both effective and sustainable.
By incorporating patient-specific factors, personalized plans can lead to improved adherence to medication regimens, reduced side effects, and enhanced patient satisfaction. This proactive approach empowers patients to actively participate in their care, fostering a stronger doctor-patient relationship built on mutual understanding and shared decision-making.
Medication Management: Optimizing Adherence and Outcomes
Effective medication management is a cornerstone of personalized treatment plans. It encompasses not only the correct dosage and timing of medications but also the patient's ability and willingness to adhere to the prescribed regimen. Understanding the potential barriers to adherence, such as cost, complexity of the medication schedule, or side effects, is vital in developing strategies to overcome them.
Tailoring Medication Regimens to Specific Needs
A key aspect of personalized medication management is tailoring the regimen to the specific needs of the individual. This includes considering factors such as age, weight, renal function, liver function, and potential drug interactions. Adjusting dosages and selecting appropriate formulations can significantly impact the efficacy and safety of treatment.
Monitoring and Adjusting Treatment Based on Response
Personalized treatment plans are not static; they require ongoing monitoring and adjustments based on the patient's response to treatment. Regular check-ups, blood tests, and other assessments allow clinicians to track progress, identify any emerging issues, and make necessary modifications to the plan. This dynamic approach ensures that the treatment remains effective and safe throughout the course of care.
Patient Education and Empowerment: Active Participation in Care
Patient education plays a vital role in personalized treatment plans. Educating patients about their condition, medications, potential side effects, and lifestyle modifications empowers them to actively participate in their care. This active involvement fosters a collaborative partnership between the patient and healthcare team, leading to better outcomes and improved adherence to the treatment plan.
Integrating Technology for Enhanced Medication Management
Technological advancements offer significant opportunities to enhance medication management within personalized treatment plans. Mobile apps, wearable devices, and electronic health records can help patients track their medication intake, monitor their health, and communicate effectively with their healthcare providers. This integration of technology facilitates better adherence, improved outcomes, and a more convenient and efficient healthcare experience.
Emotional eating, a common coping mechanism, involves using food to manage difficult emotions like stress, anxiety, or sadness. This often results in overeating and can lead to a range of health problems. Understanding the underlying emotional triggers is crucial for developing healthy coping strategies. Identifying these triggers, whether it's boredom, loneliness, or anger, can help individuals find more constructive ways to deal with their feelings. It's important to acknowledge that emotional eating isn't inherently bad; it's a learned behavior that can be unlearned with the right support and strategies.
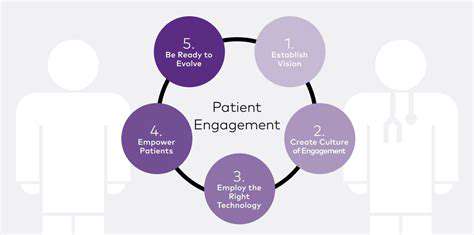
Enhancing Communication and Support: Bridging the Gap Between Patients and Caregivers
Improving Patient Understanding
Effective communication is paramount in healthcare, and ensuring patients understand their conditions, treatment plans, and potential side effects is crucial. Clear, concise explanations, tailored to the individual's comprehension level, are essential. This includes providing readily accessible information in multiple formats, such as written materials, videos, and interactive tools. Furthermore, actively encouraging questions and addressing concerns promptly and thoroughly can significantly improve patient understanding and engagement in their care.
Facilitating open dialogue between healthcare professionals and patients is key. Active listening, empathy, and a genuine interest in the patient's perspective can foster trust and rapport, ultimately leading to a shared understanding of the patient's needs and goals for treatment. This approach not only improves patient outcomes but also enhances the overall quality of care.
Building Strong Caregiver Support Networks
Caregivers play a vital role in the healthcare journey of patients, often facing significant emotional and practical challenges. Providing robust support networks for caregivers is essential to alleviate stress and burnout. This includes offering educational resources, practical guidance on caregiving tasks, and opportunities for caregivers to connect with others facing similar experiences. Support groups, workshops, and online forums can all contribute to a sense of community and shared understanding.
Developing Effective Communication Strategies
Clear and consistent communication between patients, caregivers, and healthcare providers is fundamental to successful care. Establishing clear communication channels and protocols, such as regular check-ins, scheduled updates, and accessible contact information, is crucial. This ensures that everyone involved is informed and involved in the decision-making process. Using technology to facilitate communication, such as secure messaging platforms or telehealth tools, can further streamline information flow and improve accessibility.
Addressing Cultural and Linguistic Barriers
Cultural and linguistic differences can significantly impact communication and support. Healthcare professionals need to be culturally competent and sensitive to diverse backgrounds, ensuring that communication methods are appropriate and respectful of cultural norms. Utilizing interpreters, providing multilingual resources, and offering culturally relevant support services can effectively bridge these gaps and promote inclusivity in healthcare.
Empowering Patients and Caregivers
Empowering patients and caregivers through education and information empowers them to actively participate in their care. Providing access to reliable resources, such as patient portals, educational materials, and online support groups, fosters a sense of autonomy and control. This empowers patients and caregivers to make informed decisions, ask questions, and advocate for their needs. Encouraging self-management strategies and empowering patients to take ownership of their health can lead to better outcomes.
Utilizing Technology for Enhanced Support
Modern technology offers powerful tools to enhance communication and support within healthcare. Utilizing telehealth platforms, secure messaging systems, and patient portals can streamline communication and provide convenient access to information and support. These technologies can facilitate remote monitoring, virtual consultations, and access to educational materials, ultimately bridging geographical barriers and improving the overall patient experience. The use of these technological advancements can also reduce wait times and increase the efficiency of care delivery.
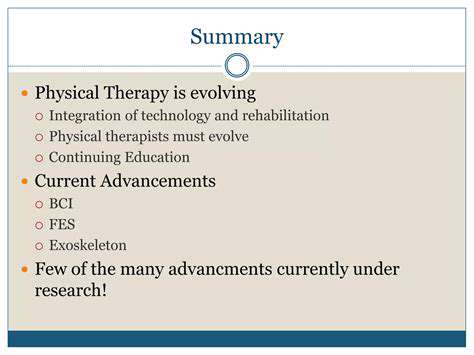
The Future of Geriatric Care: Ethical Considerations and Practical Implementations
Ethical Considerations in Long-Term Care
The future of geriatric care hinges significantly on addressing ethical dilemmas surrounding end-of-life decisions, advanced directives, and the allocation of resources. Ensuring dignity and autonomy for elderly patients is paramount, requiring a nuanced understanding of their values and preferences, even in situations of declining capacity. Care providers must navigate complex situations with sensitivity and respect, prioritizing the well-being and wishes of each individual within the framework of ethical principles and legal guidelines.
This involves robust discussions about the quality of life, the patient's goals, and the potential burdens of treatment. Ethical frameworks must be adaptable to the diverse needs and perspectives of older adults from different cultural backgrounds and socioeconomic situations. This adaptability is crucial for equitable access to high-quality care and respect for individual choices.
Technological Advancements in Care Delivery
Technological advancements are poised to revolutionize the delivery of geriatric care, potentially improving efficiency, accessibility, and quality. Remote monitoring systems, telemedicine platforms, and AI-powered diagnostic tools can enhance the ability to provide timely and personalized care, even in remote or underserved areas.
These innovations hold significant potential for reducing hospital readmissions, improving patient outcomes, and ultimately, boosting the overall quality of life for older adults. However, the ethical implications of these technologies, including data privacy and security, must be carefully considered and addressed.
Financial Sustainability of Care Systems
The aging global population presents a considerable challenge to the financial sustainability of geriatric care systems. As the number of older adults increases, the demand for long-term care services, skilled nursing facilities, and home healthcare will surge. This necessitates innovative strategies for funding and resource allocation, potentially involving partnerships between public and private sectors.
Interdisciplinary Collaboration and Care Coordination
Effective geriatric care necessitates strong interdisciplinary collaboration. Physicians, nurses, social workers, therapists, and family members must work together to provide comprehensive care that addresses the physical, emotional, and social needs of older adults. This collaborative approach is crucial for ensuring that patients receive holistic and individualized care that meets their unique needs and preferences, ultimately promoting their well-being.
Community-Based Support Systems
Robust community-based support systems are essential for providing comprehensive geriatric care. These systems can encompass a range of services, from transportation assistance and meal delivery to social activities and volunteer programs. This approach fosters a sense of community and belonging for older adults, thus improving their overall well-being and encouraging independence. These support systems are vital for reducing social isolation, promoting mental wellness, and maintaining a high quality of life.
Training and Education for Healthcare Professionals
Continuous training and education are crucial for healthcare professionals who work with older adults. This includes specialized training in geriatric care, palliative care, and end-of-life decision-making. Healthcare professionals need to be equipped with the knowledge, skills, and emotional intelligence necessary to provide compassionate and effective care to the elderly. This continuous learning and development will be essential for adapting to the evolving needs of an aging population and fostering a supportive care environment.
Patient Empowerment and Active Participation
Patient empowerment and active participation are crucial components of high-quality geriatric care. Older adults should be actively involved in decisions regarding their care, treatment, and future planning. Encouraging open communication, shared decision-making, and fostering a sense of control over their lives can significantly enhance the quality of their experiences. This empowerment also contributes to a better understanding of individual preferences and goals, leading to more effective and satisfying care arrangements.