Navigating the Complex Healthcare System
Patient navigation plays a crucial role in helping individuals navigate the often-complex and overwhelming healthcare system. This involves understanding the various services available, insurance coverage, and the different steps involved in receiving appropriate care. Effectively navigating this system can significantly improve patient outcomes and reduce the stress associated with illness or injury. Patients who feel lost or confused are more likely to experience delays in care, leading to potentially worse health outcomes.
A well-trained patient navigator can act as a trusted guide, providing clear and concise information about the patient's specific needs and options. This includes understanding the patient's financial limitations, cultural sensitivities, and personal preferences in order to provide the best possible support.
Empowering Patients Through Information
A key element of patient navigation is empowering patients with the knowledge and resources they need to make informed decisions about their health. This includes providing access to accurate information about their diagnosis, treatment options, and potential side effects. Providing this information in a clear and compassionate manner is essential for fostering trust and collaboration between patients and healthcare providers.
Furthermore, patient navigation programs can equip patients with the tools to actively participate in their own care, such as understanding their medication regimens, scheduling appointments, and advocating for their needs.
Improving Access to Care for Vulnerable Populations
Patient navigation is particularly important for vulnerable populations who face significant barriers to accessing healthcare. These barriers can include socioeconomic factors, language barriers, cultural differences, or geographic limitations. By addressing these specific needs, patient navigation can help bridge these gaps and improve equity in healthcare access.
Patient navigators can provide culturally sensitive support, assist with language interpretation, and connect patients with community resources, ensuring that no one is left behind in the pursuit of better health outcomes.
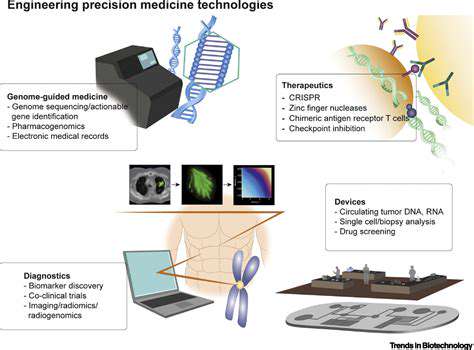
Technological Advancements in Patient Navigation
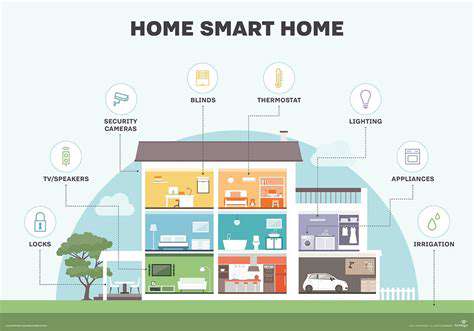
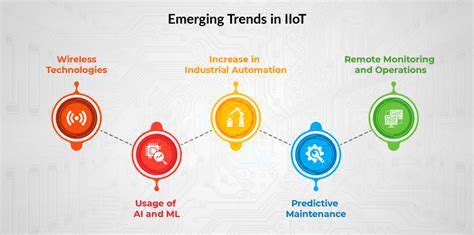
Technological advancements are revolutionizing patient navigation, creating more efficient and accessible services. Telehealth platforms, online resources, and mobile applications are enabling patients to connect with navigators remotely, enhancing convenience and accessibility. This increased accessibility is especially beneficial for individuals in rural or underserved areas who may have limited access to traditional healthcare facilities.
Collaboration and Integration with Healthcare Teams
Successful patient navigation requires strong collaboration between patient navigators, healthcare providers, and other support staff. This collaborative approach ensures that patients receive coordinated and comprehensive care. Effective communication and information sharing between these teams are crucial for seamless transitions and continuity of care.
Integrating patient navigation services into the mainstream healthcare system is essential for maximizing their impact. This integration requires clear communication channels and established processes for referring patients to navigators when necessary.
The Future of Patient Navigation: Personalized and Proactive Care
The future of patient navigation will likely emphasize personalized and proactive approaches. This means tailoring support to the specific needs and preferences of each patient, anticipating potential barriers, and intervening proactively to prevent complications. Proactive interventions can significantly improve patient outcomes by addressing potential problems before they escalate.
Utilizing predictive modeling and data analytics will allow patient navigators to identify patients at high risk and offer targeted support, ultimately improving the overall quality of care.