Improving Accuracy in Sleep Studies
AI-powered analysis of polysomnography (PSG) data holds immense potential for enhancing the accuracy of sleep diagnoses. By meticulously examining complex waveforms and patterns, AI algorithms can identify subtle indicators of sleep disorders that might be missed by human interpretation. This improved accuracy translates to more precise diagnoses, enabling clinicians to tailor treatment plans effectively and avoid misdiagnosis, which is crucial for patient well-being. The ability to detect subtle variations in brainwave activity, muscle tone, and breathing patterns, often missed by the human eye, is a significant advantage of AI in sleep studies.
Furthermore, AI algorithms can account for a wider range of data points, leading to a more comprehensive understanding of sleep patterns. This broader perspective can unveil complex interactions between various physiological parameters, providing a more nuanced view of sleep quality and potential underlying issues. Such accuracy is essential for patients with complex sleep disorders, ensuring they receive the most appropriate and effective treatment.
Automating Data Processing
One of the most significant benefits of AI in polysomnography analysis is the automation of data processing. Traditional methods involve significant manual effort in reviewing and interpreting the vast amount of data generated during a sleep study. AI algorithms can rapidly process this data, freeing up clinicians' time to focus on patient care and detailed interpretation. This automation streamlines the workflow, reducing the time spent on repetitive tasks and allowing for faster turnaround times in providing patients with results.
Enhanced Efficiency in Sleep Disorder Detection
AI can significantly accelerate the process of identifying sleep disorders. By quickly analyzing complex data patterns, AI algorithms can flag potential issues, such as sleep apnea, insomnia, or narcolepsy, for closer examination. This enhanced efficiency allows for earlier intervention, potentially improving patient outcomes and reducing the time it takes for patients to receive appropriate treatment. The ability to rapidly identify and prioritize cases saves valuable time and resources for clinicians and healthcare systems.
Minimizing Human Error
Human interpretation of polysomnography data is prone to errors, particularly when dealing with large datasets or complex cases. AI algorithms, trained on vast amounts of data, can significantly reduce the risk of human error by objectively analyzing the data without subjective biases. This objective assessment ensures consistent results, regardless of the clinician or time of day. Eliminating human error is paramount for maintaining the accuracy and reliability of sleep diagnoses.
Improved Accessibility to Sleep Diagnostics
By automating the analysis process and reducing the workload on clinicians, AI-assisted polysomnography analysis can make sleep diagnostics more accessible to a wider range of patients. This increased accessibility can lead to earlier diagnosis and treatment, particularly in underserved areas or for individuals with limited access to specialized sleep clinics. Making sleep diagnostics more readily available is crucial for improving patient outcomes and public health.
Cost-Effectiveness of AI-Based Analysis
The automation capabilities of AI can significantly reduce the overall cost of sleep studies. By minimizing the need for extensive manual review and analysis, AI-assisted analysis can lower operational costs for sleep clinics and hospitals. This efficiency translates to potentially lower costs for patients, making sleep diagnostics more affordable and accessible to a broader population. The long-term cost savings associated with AI-based analysis are substantial, impacting both healthcare providers and individuals.
Future Applications of AI in Sleep Medicine
The potential applications of AI in sleep medicine extend beyond polysomnography analysis. AI algorithms can be utilized for developing personalized sleep interventions, predicting sleep disorders, and even improving the design of sleep-promoting devices. Further research in this area will undoubtedly lead to even more innovative applications of AI in sleep medicine, ultimately revolutionizing the field and improving the quality of life for individuals with sleep disorders. The future of sleep medicine is intertwined with the advancement of AI, promising a new era of precision and personalized care.
Predictive Modeling for Early Detection and Personalized Treatment Plans

Predictive Modeling Techniques
Predictive modeling, a crucial aspect of data science, employs various techniques to forecast future outcomes based on historical data. These techniques encompass a wide array of algorithms, from simple linear regression to complex machine learning models like neural networks. Understanding the strengths and weaknesses of each technique is vital for selecting the most appropriate model for a specific problem.
A key element in choosing the right technique is the nature of the data being analyzed and the desired outcome. For example, if the goal is to predict continuous values, such as house prices, regression models might be suitable. Conversely, if the aim is to classify data into categories, like identifying spam emails, classification algorithms would be more appropriate.
Data Preparation and Feature Engineering
Before applying predictive models, careful data preparation is essential. This involves cleaning, transforming, and preparing the data to ensure its quality and suitability for analysis. Missing values need to be handled appropriately, and outliers identified and addressed. Feature engineering is also critical, as it involves creating new features from existing ones to improve model performance. This often includes transforming variables, creating interactions, or applying domain expertise.
Data preparation is often the most time-consuming part of the process but it is crucial for the success of the predictive model. Poorly prepared data can lead to inaccurate and unreliable predictions.
Model Selection and Evaluation
The selection of the appropriate predictive model depends heavily on the characteristics of the data and the specific problem. Various factors, including the type of data (numerical, categorical), the size of the dataset, and the desired level of accuracy, influence the decision. Understanding the strengths and weaknesses of different models is essential for making informed choices.
Model Training and Tuning
Model training involves using the prepared data to teach the chosen algorithm to identify patterns and relationships. This process involves feeding the model with training data and allowing it to learn the optimal parameters. Model tuning, on the other hand, involves refining the model's parameters to improve its performance on unseen data.
Interpreting Model Results
Understanding the insights derived from the model is as important as building the model itself. Interpreting the results involves analyzing the coefficients, probabilities, or other outputs to understand the factors influencing the predictions. A well-interpreted model provides valuable insights into the relationships within the data and can be used to support business decisions.
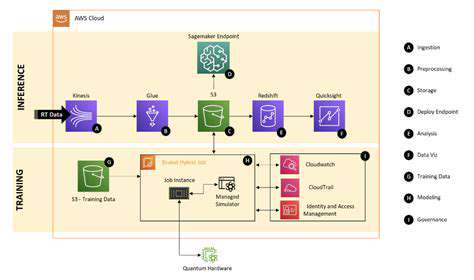
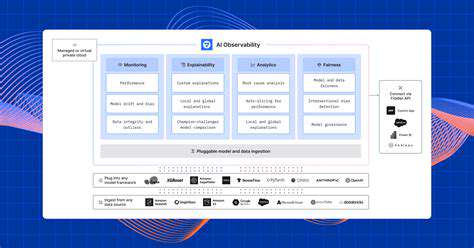
Deployment and Monitoring
Once a predictive model is deemed satisfactory, it needs to be deployed into a production environment. This involves integrating the model with existing systems and ensuring its ongoing functionality. Ongoing monitoring is crucial to detect any drift in the data or changes in the underlying relationships that might affect the accuracy of the predictions.
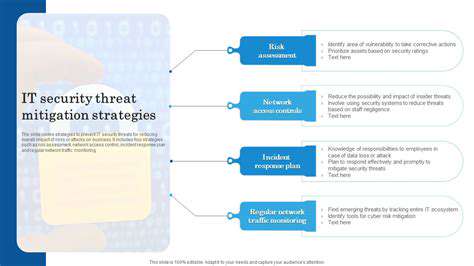
Ethical Considerations
Predictive modeling, while powerful, can raise ethical concerns. Bias in the data can lead to biased predictions, which can have significant consequences. It's essential to carefully consider the potential societal impact of the model and to ensure fairness and transparency in its development and deployment. Understanding and mitigating these biases is crucial for responsible data science practice.
Autophagy, a Greek word meaning self-eating, is a crucial cellular process essential for maintaining cellular health and longevity. It's a fundamental mechanism where cells break down and recycle damaged proteins, organelles, and other cellular components. This recycling process is vital for removing cellular waste and preventing the accumulation of harmful substances, which can contribute to various age-related diseases. This intricate process involves a complex network of cellular pathways and is tightly regulated to ensure efficient and controlled degradation.
AI-Driven Tools for Remote Patient Monitoring and Management
AI-Powered Remote Monitoring
AI-driven tools are revolutionizing remote patient monitoring by automating the collection and analysis of patient data. These tools can analyze a variety of data sources, including wearable sensor data, electronic health records (EHRs), and even voice recordings, to identify patterns and trends that may indicate potential health issues. By automating this process, healthcare providers can more effectively identify patients at risk and intervene proactively, potentially preventing serious complications.
The ability to process large volumes of data quickly and accurately is a significant advantage of these AI-powered tools. This allows for personalized care plans and real-time adjustments based on the evolving health status of the patient. These tools are crucial in enabling continuous monitoring, especially for patients with chronic conditions, enabling early detection of deterioration and facilitating timely interventions.
Predictive Analytics for Health Outcomes
AI algorithms can analyze historical patient data to predict future health outcomes. This predictive capability allows healthcare providers to identify patients who are at high risk for developing specific conditions, enabling proactive interventions and potentially improving patient outcomes. These predictions can be used to tailor preventative care strategies and provide early interventions that can significantly impact health outcomes.
By identifying patterns and trends in patient data, AI can flag potential risks and provide early alerts to healthcare providers. This proactive approach can significantly improve the quality of care and reduce the likelihood of adverse events. Early intervention is often key to mitigating complications and improving patient well-being.
Personalized Treatment Plans
AI-driven tools can analyze individual patient data to create personalized treatment plans. This includes considering factors like age, genetics, lifestyle, and medical history to develop a tailored approach to care. These personalized plans can lead to improved treatment adherence and better health outcomes for patients.
Improved Efficiency and Cost-Effectiveness
AI-driven tools can streamline various aspects of remote patient care, leading to improved efficiency and cost-effectiveness for healthcare systems. By automating tasks such as data collection, analysis, and report generation, these tools can free up healthcare providers' time to focus on more complex patient interactions and care management. This increased efficiency can translate into significant cost savings for healthcare systems, allowing for better allocation of resources and investment in other areas of patient care. The ability to predict potential issues and intervene early also reduces the need for costly hospitalizations and emergency room visits.
The Future of AI in Sleep Medicine: Challenges and Opportunities
Improving Diagnostic Accuracy
AI algorithms can analyze sleep data with unprecedented precision, identifying subtle patterns indicative of sleep disorders that might be missed by traditional methods. This enhanced diagnostic capability translates into earlier intervention and more accurate diagnoses, ultimately leading to better patient outcomes. By leveraging machine learning models trained on massive datasets of sleep recordings and associated clinical data, AI can potentially distinguish between various sleep disorders, such as insomnia, sleep apnea, and narcolepsy, with higher accuracy and speed than human clinicians alone.
Furthermore, AI can also help to identify risk factors for sleep disorders, allowing for proactive interventions and potentially preventing the onset of these conditions. This proactive approach is crucial for improving public health and reducing the burden of sleep-related illnesses.
Personalized Treatment Plans
AI can tailor sleep therapy strategies to individual patient needs. By analyzing a patient's unique sleep patterns, medical history, and lifestyle factors, AI can recommend personalized treatment plans that are more effective and less prone to side effects compared to generic approaches. This personalized approach can significantly improve patient compliance and treatment outcomes.
For instance, AI can adjust the intensity and duration of therapies like CPAP for sleep apnea, dynamically adapting to the patient's changing respiratory patterns throughout the night. This adaptability is key to optimizing treatment efficacy and minimizing discomfort for patients.
Enhanced Monitoring and Remote Patient Management
AI-powered wearable devices and home monitoring systems can continuously track sleep data, providing real-time insights into patients' sleep quality and patterns. This continuous monitoring allows for early detection of changes in sleep patterns, enabling proactive interventions and adjustments to treatment plans. The ability to monitor patients remotely can significantly improve access to care, particularly for individuals in underserved areas or those with mobility limitations.
Addressing Data Bias and Ensuring Ethical Considerations
The effectiveness of AI models in sleep medicine hinges on the quality and representativeness of the training data. Addressing potential biases in these datasets is crucial to ensure equitable and unbiased applications of AI in sleep medicine. Bias in data can lead to inaccurate diagnoses and unequal access to effective treatments. Therefore, careful consideration of data diversity and the development of robust methodologies to mitigate bias are essential for responsible AI deployment.
Advancements in Sleep Research
AI can accelerate sleep research by enabling faster and more comprehensive analysis of large datasets. This capacity allows researchers to explore complex relationships between sleep, health, and other factors, leading to groundbreaking discoveries about sleep mechanisms and their impact on overall well-being. AI can also identify new patterns and correlations in sleep data that might be missed by traditional approaches, opening up exciting avenues for future research and discoveries.
Cost-Effectiveness and Accessibility
AI-powered sleep diagnostics and treatment solutions have the potential to significantly reduce healthcare costs. By automating tasks, improving diagnostic accuracy, and enabling remote monitoring, AI solutions can streamline workflows and reduce the need for extensive in-person visits. This cost-effectiveness can make sleep medicine care more accessible to a wider range of patients, particularly those with limited access to specialized care.
Improving Sleep Hygiene Education
AI can analyze data on sleep hygiene practices to identify common patterns and areas for improvement. This can lead to the development of more effective and personalized sleep hygiene recommendations. AI can also facilitate the delivery of educational resources about sleep hygiene, making information more accessible and engaging for patients. This proactive approach can empower individuals to take control of their sleep health and prevent future sleep disorders.