Post-Surgical Monitoring: Technological Advancements
The field of post-surgical monitoring is rapidly evolving, driven by advancements in technology. These advancements promise to revolutionize patient care by enabling more precise and proactive interventions, ultimately leading to improved patient outcomes and reduced hospital stays. Sensors and wearable devices are becoming increasingly sophisticated, allowing for continuous and real-time data collection, which can be invaluable in identifying potential complications early on.
From sophisticated physiological monitoring to early warning systems, the shift toward proactive and personalized care is evident. This increased monitoring allows for faster identification of potential problems, facilitating timely interventions and minimizing the risk of adverse events.
Real-Time Data Collection and Analysis
Real-time data collection and sophisticated analytics are transforming post-surgical monitoring. By continuously monitoring vital signs and other relevant parameters, medical professionals can identify subtle changes that might indicate developing complications, allowing for prompt intervention and potentially preventing serious issues.
The ability to analyze this data in real-time enables proactive adjustments to treatment plans, leading to more personalized and effective care. This data-driven approach to post-surgical care is poised to significantly improve patient outcomes and reduce the overall cost of healthcare.
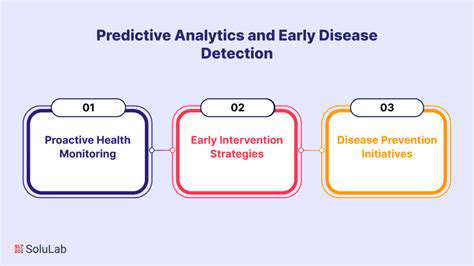
Early Warning Systems and Predictive Modeling
Early warning systems, powered by algorithms trained on vast datasets, are becoming increasingly sophisticated. These systems can identify patterns and predict potential complications before they manifest, allowing for proactive interventions. This proactive approach is crucial in minimizing the risk of adverse events.
Sophisticated predictive models are also being developed, utilizing machine learning to anticipate potential complications and tailor treatment plans accordingly. This personalized approach is leading to more effective and efficient post-surgical care.
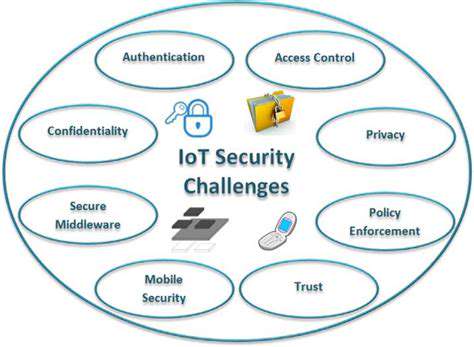
Remote Patient Monitoring: Expanding Access and Convenience
Remote patient monitoring (RPM) is expanding access to post-surgical care and enhancing patient convenience. Patients can be monitored in their homes, allowing for continuous data collection and real-time communication with healthcare providers. This remote monitoring fosters greater patient autonomy and empowers them to actively participate in their recovery.
The ability to monitor patients remotely is particularly valuable for those in underserved areas, enabling access to specialized care that might otherwise be unavailable. This expands the reach of high-quality post-surgical care, improving health equity.
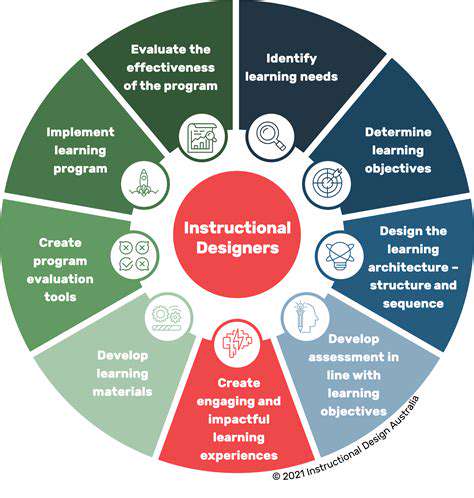
Personalized Treatment Plans: Tailoring Care to Individual Needs
Post-surgical monitoring data is instrumental in creating personalized treatment plans. By analyzing individual patient responses to various interventions, healthcare providers can tailor care to specific needs, optimizing recovery and improving overall outcomes. This personalized approach leads to a greater sense of patient control and empowers them in their journey of recovery.
Individualized care strategies are vital for optimizing outcomes and minimizing the potential for adverse events. This data-driven approach to care allows for the most effective treatment strategies to be developed for each patient.
Integration of Wearable Technologies
The integration of wearable technologies into post-surgical monitoring is revolutionizing the way patients are cared for. These devices provide continuous monitoring of vital signs, activity levels, and other important parameters, offering valuable insights into patient recovery. This continuous monitoring provides an invaluable level of detail for healthcare professionals, allowing them to intervene more effectively.
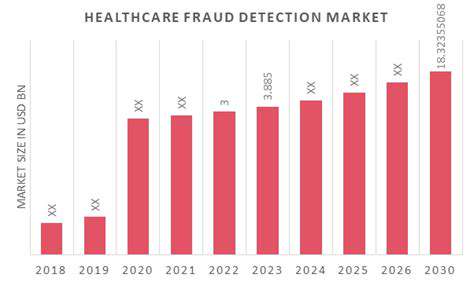
Cost-Effectiveness and Efficiency Improvements
Improved post-surgical monitoring systems are expected to lead to significant cost savings and greater efficiency in healthcare delivery. By reducing hospital readmissions and length of stay, these systems can lower overall healthcare costs while simultaneously improving patient outcomes. This translates into substantial financial savings for healthcare systems, which can then be reinvested in further advancements and improvements.
The ability to identify and address potential complications early on through real-time monitoring translates directly into reduced resource utilization, leading to greater overall efficiency within the healthcare system.